Abstract
Introduction: Therapy-related acute myeloid leukemia (t-AML) covers a poorly defined group (grp) of patients (pts) who develop AML following cytotoxic or radiation therapy. Most pts have a prior malignancy but 5-20% have exposure to cytotoxic therapy for benign disorders, such as autoimmune diseases (AD). The aim of this study was to define the characteristics, mutational profiles and outcomes of pts with AD and AML.
Methods: Pts with AML diagnosed from 1999-2017 were identified and divided into 4 grps: de novo AML, AML with a prior history of AD (AD-AML), t-AML excluding AD-AML, and AML evolving from antecedent myelodysplastic syndrome (MDS) or other myeloid stem cell disorders without prior history of AD (s-AML). Molecular data were obtained using different platforms of next generation sequencing (NGS) of genes that are known to be commonly mutated in AML (number of covered genes varied from 37 - 60). Categorical data were analyzed using Fisher's exact test for 2-grp comparisons of categorical data with 2 levels; chi-square tests for comparisons of categorical data involving >2 grps and/or factors with >2 levels; t-tests and ANOVA were used for comparisons of continuous factors, and the log rank test was used for comparisons of overall (OS) and relapse-free survival (RFS).
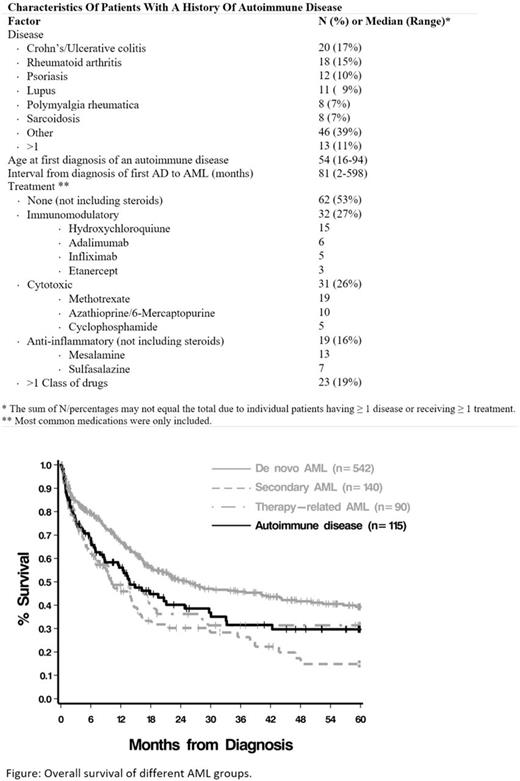
Results: A total of 910 pts were included: 13% (n=118) with AD-AML, 60.7% (n=553) de novo AML, 16% sAML (n=146) and 10.2% t-AML (n=93). Median age at diagnosis was 63 years; 55% were male; 66% received intensive induction therapy. Cytogenetic data were available for 94% of pts and, according to MRC 2010 classification, were favorable in 16%, intermediate in 56% and poor in 29% of the pts. Most prevalent AD were Crohn's/ulcerative colitis (n=20, 17%), rheumatoid arthritis (n=18, 15%), psoriasis (n=12, 10%), and lupus (n=11, 9%); 11% of pts had 2 disorders (Table). Median age at diagnosis of first AD was 54 years (range 16-94) and median interval from AD diagnosis to AML was 81 months. The majority of pts (53%) did not receive treatment (not including steroids) for their AD. 27% of pts were treated with immunomodulating agents, 26% with cytotoxic agents and 14% with anti-inflammatory agents; 19% received ≥ 2 drug classes. Poor risk cytogenetics were more common in AD-AML than in de novo AML (37% vs. 22%, p=.0003), which was driven mainly by chromosome 7 (19% vs. 9%, p=.004) and 17 (11% vs. 5%, p=.01) abnormalities. NGS data were available for 338 pts, of whom 40 had AD-AML. Mutations in SRSF2 were more common in AD-AML (23%) than in de novo (10%, p=.03) and sAML (7%, p=.03). In pts with sAML arising from MDS/myeloproliferative disorders (MPN) and available NGS data (n=82), SRSF2 mutations were more common in pts with AD (5/16, 31%) versus non-AD (4/66, 6%; p=.01). Compared with t-AML, pts with AD-AML had more frequent mutations in NPM1 (18% vs. 0%, p=.03) and NRAS (15% vs. 0%, p=.03). Overall, mutations in signaling pathways were more common in pts with AD-AML (55% vs. 36%, p=.03), while mutations in genes involved with histone and chromatin modification were less common (7% vs. 20%, p=.04). Rate of complete remission and RFS were similar among de novo (71%, 15 months), AD-AML (68%, 13 months) and t-AML (68%, 13.5 months) groups. For the AD-AML grp, the median OS was 16 months; significantly shorter compared with de novo AML (25 months, p=.02), and similar to t-AML (10 months, p=.71) and sAML (10 months, p=.14) (Figure).
Conclusion: Patients with AML and a prior history of AD have cytogenetic profile and outcomes similar to those with t-AML but with distinct molecular features. In pts with MDS/MPN transformed into AML, SRSF2 mutations are more common in those with history of AD. These findings need to be validated in large series; however, they suggest that spliceosome inhibitors might be a future focus of investigation in pts with AD-AML.
Gerds: CTI BioPharma: Consultancy; Incyte: Consultancy. Sekeres: Celgene: Membership on an entity's Board of Directors or advisory committees. Advani: Takeda/ Millenium: Research Funding; Pfizer: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal